Physiotherapy is an evidence-based rehabilitation science that combines the knowledge of anatomy, kinesiology, physiology and neuroscience to assess, diagnose, treat, and plan the management of acute and chronic injuries/conditions, mobility impairments, pain, and women’s and men’s pelvic health conditions (to name a few!). We also work with individuals who want to optimize athletic performance and skill. Using a client-centered approach to help you achieve your goals, we are here to help you participate to your fullest in life!
Our Physiotherapy treatments include:
- Acupuncture/Dry Needling
- Clinical Pilates
- Concussion Rehab
- Manual Therapy
- Orthopaedic injuries and Arthritis care
- Pelvic Floor Physiotherapy
- Shockwave Therapy
- TMJ Disorders
Bracing & Taping
Orthopaedic bracing/splinting

Brace fitting is required prior to placing orders and can be done within the scope of a physiotherapy visit.
Trusted and well respected brands we carry
- AIRCAST
- ASO
- ASPEN QUICK DRAW
- BAUERFIEND/epitrain
- BREGG
- OSSUR
- OTHER: by request
Taping

Clinical Pilates
What are Pilates Exercises?
Pilates is form of exercise that focuses on improving core stability, postural alignment, mobility, coordination and balance; and gives important consideration to breathing awareness during movement. It was developed by Joseph Pilates, a pioneer of his time, and monumentally ahead of his cultural era in terms of physical fitness and conditioning. The Pilates method was born from Joseph’s dedication to understand human anatomy and movement, and to improve his own physical fitness in a balanced way. He called his method “Contrology”, and advocated it as an all encompassing movement form that unites spirit, mind, and body.
Through his method Joseph became an accomplished athlete, performer, and trainer/rehabilitation professional to war veterans, police, and athletes such as boxers and dancers. His method has been carried on for years past his death in 1967, and saw a major surge in the fitness industry starting in the 1980’s. Today, Pilates exercises continue to be a widely practiced movement form for people of all ages and abilities, and with different physical goals in mind.
What is Clinical Pilates?
Clinical Pilates is the teaching of the Pilates method exercises by a medical professional, such as a physiotherapist in order to assist with a client’s rehabilitation. Pilates can be safely applied to most rehabilitation needs and modified according to a client’s limitations. Once a physiotherapist has assessed the client and determined their physical needs in combination with the client’s goals a therapeutic exercise program of Pilates can be prescribed and taught.
Clinical Pilates Can Help With The Following Conditions.
- weak core muscle strength
- postural faults
- impaired balance
- spinal pain and dysfunction
- impaired flexibility
- prenatal fitness and postpartum recovery
Lina and Rachel are both trained in Mat and Reformer Pilates.
Concussion Rehabilitation
Claire McDonald is our resident physiotherapist who has additional training in concussion rehabilitation, she is available both in-person and online via telehealth for concussion assessment and treatment.
What is a concussion?
A concussion is an acute neurophysiological event induced by traumatic biomechanics forces to the head, neck or body as a result of sudden acceleration, deceleration or rotational force. This trauma will result in a set of clinical symptoms that may or may not include a loss of consciousness.
A concussion can be sustained from:
- a motor vehicle crash
- sport or recreational injury
- falls
- workplace injury
- assault
The majority of sport-related concussions resolve in 7-10 days from onset, but symptoms that surpass beyond the natural recovery period are classified as post-concussion syndrome.
What are the symptoms of concussion?
- Headache
- Dizziness/Vertigo
- Fatigue
- Brain fog/cognitive challenges
- Sleep disturbances
- Vision changes, such as light sensitivity
- Noise sensitivity
- Behavioural changes, such as irritability
- Anxiety, depression and changes in mood
There is no one-size-fits-all for concussion care, as every patient presents with different clinical signs and symptoms. Concussion treatment options may include:
- vestibular-ocular rehabilitation
- cardiovascular training
- dynamic and static postural stability
- cervical spine biomechanics and kinesthetic function
- education and activity planning and pacing
- return to sport/activity
Claire McDonald is our resident physiotherapist who has additional training in concussion rehabilitation, she is available both in-person and online via telehealth for concussion assessment and treatment.
Dry Needling

Medical/Anatomical Acupuncture is a dry needling technique that applies the principles of Traditional Chinese Medicine blended with Western Medicine. Traditional acupoints are used to relieve pain and inflammation in tissues that have been injured. The approach is based on the anatomical location of the injury or pain by using acupoints that relate to the joint(s), ligament(s), muscle(s) and nerve(s) of that area.
Chris, Claire, Lina and Rachel have credentialing in Dry Needling techniques. Claire and Rachel are both certified in acupuncture through the Acupuncture Foundation of Canada Institute, a foundation and teaching model developed by Dr. Joseph Wong.
Exercise Prescription & Conditioning
Therapeutic Exercises or Sports Specific Conditioning:
Can be prescribed to help rehabilitate injury, prepare for surgery, or achieve athletic goals. Exercise prescription can be provided during treatment sessions in clinic for clients who will take them home to perform either there or at their gym. Otherwise, the physiotherapist can arrange to meet the client at their gym of choice to receive their program and orient them to the equipment.
Chronic Disease Management:
Exercises can be prescribed based on current research evidence for people with conditions such as arthritis, cardiac, chronic pain, inflammatory/rheumatic diseases, metabolic (Diabetes), and neurological management (MS, Parkinson’s, Stroke).
Exercise prescription can include a combination of the following:
- Agility and coordination training
- Cardiovascular fitness
- Core stabilization
- Flexibility
- Motor recruitment patterning and retraining
- Muscular endurance, strength, or power
- Proprioceptive training/balance
Exercise equipment can include a combination of the following:
- Balance boards
- Body weight/gravity
- Cardio machines
- Exercise balls
- Foam rollers
- Free weights
- Massage balls
- Machine weights
- Medicine balls
- Pulleys
- Steps/ boxes
- Therapeutic resistance bands
- Your own free will
Manual Therapy
Manual therapy is a hands on approach to help release tight muscles, restricted joints, and scar tissue in order to regain full range of motion, reduce pain, and improve overall mobility and function.
Types of manual therapy include:
Deep Frictions: pressure applied perpendicular to the tissue fibers to bring circulation, reduce pain, and help connective tissue realign for injured tendons, ligaments, and muscle.
Joint Manipulation/Mobilization: Joint manipulations are rapid movements at a joint’s end range to help quickly release restricted areas and restore movement. Joint mobilizations are graded gliding of a restricted joint to help it ease into its full range of movement. Both techniques help reduce pain and bring circulation to the restricted area while restoring movement.
Soft tissue release/massage: kneading, and applying pressure through tight muscles and trigger points or fascia in order to help tissue to soften and relax.
Scar mobilization: scar tissue can reduce your mobility, especially if the skin has adhered to the connective tissue below it there will be restrictions and possibly pain from superficial nerves in the area. Progressive pressure applied to the area in various directions can help improve movement, similar to techniques used in Soft Tissue Release as described above.
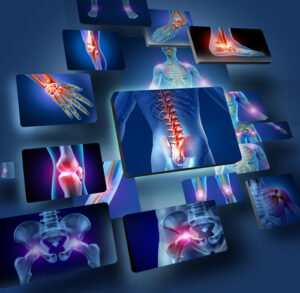
Orthopaedics
Physiotherapy assessment and treatment is beneficial for rehabilitation and recovery after soft tissue/nerve injury, as well as injury to bones and joints. Here are some of the common conditions treated in physiotherapy practice:
Head/Face/Neck: Arthritis, Bell’s Palsy, cervicogenic headaches, disc bulges/herniations, facial pain, fractures, jaw dysfunction, neck stiffness, pinched/entrapped nerve, tension headaches, trigeminal neuralgia, whiplash disorder
Shoulder: A/C joint separation, arthritis, bursitis, dislocation, frozen shoulder, joint replacement, tendon impingement, postoperative repairs, rotator cuff injury
Elbow: arthritis, biceps strain, dislocation, fractures, Golfer’s elbow (medial epicondylitis), Radial tunnel syndrome, sprains, Tennis elbow (lateral epicondylitis), triceps strain, ulnar nerve entrapment.
Wrist/Hand: arthritis, carpal tunnel syndrome, sprains, post immobilization stiffness, TFCC, tendonitis/tenosynovitis, trigger finger.
Spine: arthritis, degenerative disc disease, disc bulge/herniations, facet joint syndrome, fractures, mechanical back pain, muscle strain, rib malalignment, sciatica, scoliosis, spondylosis, spondylolisthesis, stenosis, thoracic outlet syndrome.
Pelvis: adductor strain, arthritis, fracture, hamstring strain, Osteitis Pubis (pubic symphysis pain), pregnancy related pelvic pain and hypermobility, Sacroiliac joint dysfunction, sacroiliitis.
Hip/Thigh: arthritis, bursitis, femoral nerve entrapment, fracture, gluteal pain, groin strain, hamstring strain, hipflexor strain, hip joint replacement, piriformis syndrome, quadriceps strain.
Knee/Leg: ACL rupture/reconstruction, arthritis, Baker’s cyst, bursitis, chondromalacia patella, compartment pain, fractures, knee joint replacement, LCL/MCL/PCL sprains, Meniscus tears/repairs, Osgood Schlatter’s, Patella Femoral Pain Syndrome, Patellar tendonitis, Pes Anserine syndrome, Quadriceps strain, Quadriceps tendonitis, tendon injuries to calf muscles and hamstrings.
Ankle/Foot: Achilles’ tendonitis, arthritis, bunion, excess pronation/arch drop, fractures, hallux valgus, hammer toes/flexion deformity, metatarsalgia, midfoot pain, Morton’s neuroma, muscle strains, peroneal tendonitis, plantar fasciitis, post immobilization stiffness, sprains, tibialis posterior tendonitis.
Pelvic Health for Men
Rachel Richards is trained in both pelvic floor physiotherapy for men and women.
Pelvic health is important for men too. Physiotherapy can help men recover their pelvic health through pelvic floor rehabilitation and other therapies.
Men’s Pelvic Conditions that we treat in our clinic:
- Bladder Control/Incontinence
- Bowel Constipation/Incontinence
- Coccydynia/Tailbone Pain
- Pelvic girdle pain (e.g., hips, pubic symphysis, SI joints, sacrum, coccyx)
- Pelvic Organ Prolapse
- Pudendal Neuralgia
Men’s Urinary Incontinence Solutions
Urinary incontinence can leave you avoiding activities or with feelings of isolation and depression. Despite the serious impacts that urinary incontinence has on an individual’s life, many men do not explore the variety of options available to them to lessen this impact.
LivWell Squamish can explore with you the many options that are available to help you regain the freedom you had before experiencing urinary incontinence.
Control Bladder Incontinence in Men with Contino®
Bladder incontinence is a common side-effect of prostate treatments related to prostate cancer, Benign Prostatic Hyperplasia – BPH (enlarged prostate) and Prostatitis (prostate inflammation), and can have a significant impact on your quality of life.
Contino® is an easy-to-use urethral insert that can control the flow of urine. It can be removed and re-inserted as many times a day as needed. Users report that it is painless to insert and that it allows them to return to what life was like before they experienced urinary incontinence. Users find that it reduces or eliminates the need for pads, surgical intervention, and collection devices. It is also not associated with skin irritation.
As a Contino® Authorized Trainer, LivWell Squamish can complete an independent assessment and, if appropriate, provide a personalised fitting and support of Contino®.
If your Contino® Authorised Trainer determines Contino® is right for you, you’ll get started with a 30-day trial for a fully-refundable deposit of $100. After that, a Contino® subscription delivers products straight to your door for $100 a month
Visit mycontino.com to see if Contino® is right for you and how it works, or watch this video to learn about what it’s like to use Contino®.
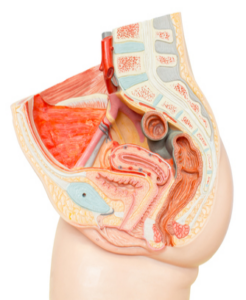
Pelvic Health for Women
Physiotherapy treatment for the following conditions is offered (listed alphabetically):
- Bladder Control/Incontinence
- Bowel Constipation/Incontinence
- Coccydynia/Tailbone Pain
- Episiotomy scar mobilization/release
- Painful Intercourse/Dyspareunia
- Pelvic girdle pain (e.g., hips, pubic symphysis, SI joints, sacrum, coccyx)
- Pelvic Organ Prolapse
- Prenatal and Postpartum health/rehabilitation
- The Four V’s: Vulvodynia, Vestibulitis, Vestibulodynia, Vaginismus (pain in the external genital tissues, at the entrance of the vagina, in the perineal area, and in the vagina).
Both Claire McDonald and Rachel Richards are trained in pelvic floor rehabilitation for women
What is Shockwave Therapy?
Shockwave therapy is a pressure wave that is transmitted through a probe into a chronically injured or painful area on the body to help it heal. It causes blood to flow to the area and stimulates more vessels to grow. It also causes a cellular cascade to provide pain relief, initiate healing, and help your cells create more healthy tissue to lay down. This technology is also applied to reducing kidney stones, called lithotripsy, when applied to musculoskeletal conditions it is termed orthotripsy.
There is currently a significant amount of research showing the effectiveness of shockwave as a non-surgical means of helping many chronic conditions to heal, provide pain relief, and improved function. See the list of treatable conditions below.
Treatable Conditions For Shockwave Therapy:
- Achilles tendinitis
- Adhesions
- Bursitis
- Calcific tendonitis or Calcific deposits
- Frozen Shoulder
- Golfer’s elbow
- Hamstring tendinitis
- Heel Spurs
- Heterotopic Ossification
- Iliotibial (I.T) band syndrome
- Metatarsal Pain
- Muscle Strains
- Osteoarthritis Pain
- Patellar tendinitis
- Plantar fasciitis
- Pubic Symphysis pain
- Rotator Cuff Tendinitis
- Scar tissue
- Shin Splints
- Tendinitis
- Tennis Elbow
- Trigger point therapy
Conditions NOT Eligible TO Use Shockwave Therapy:
If you have any of the following conditions, it is not safe for you to have Shockwave Therapy:
- Bleeding Disorder
- Blood Thinning Medication
- Cancer or Local Malignancy
- Cortisone Injection less than 6 weeks ago
- Diabetes with Neuropathy
- Inflammatory Joint Disease
- Pacemaker
- Pregnancy
NOTE: Children may have shockwave, however not near the growth plates of any bones/joints.
For safety reasons Shockwave is NOT applied over the front of the neck, chest, or abdomen, and cannot be applied over open wounds or infections.
TREATMENT PLAN:
Research suggests for most conditions 3 – 5 visits are required, each spaced 1 week apart. Some very longstanding conditions may require a few additional treatments. Initial appointments are 30 minutes, follow up appointments are usually 20 minutes. This treatment is covered under physiotherapy service for extended health plans.
Is Shockwave therapy painful?
Some people feel mild discomfort with Shockwave, but the pressure can be adjusted to a comfortable level. Usually people find it relieves their pain, even during treatment. On the rare occasion people can have slight bruising, swelling or skin redness.
What to do after a shockwave therapy treatment?
Activity and exercise as usual. Shockwave induces healing, inflammation is first stage of healing, so researchers advise not use any anti-inflammatory drugs or ice after treatment because this can reduce the effectiveness of the therapy. If you happen to have any pain it is advised to use an alternate pain relieving medication and or heat.
TELEHEALTH
Online Sessions
TELEHEALTH Online Sessions are now available for most orthopaedic and pelvic health conditions, allowing you to remain in the convenience of your current location while still receiving care! All online sessions occur through video conferencing and include assessment and treatment plans, and may use exercise programs, self mobilization/release options, corrective taping, prenatal, postnatal and all forms of pelvic health guidance.
Direct billing for TELEHEALTH sessions is available through Sun Life, Canada Life/Great West Life, and Blue Cross providers. Billing for ICBC available for subsequent visits only.
Who can use Telehealth Physio services?
Telehealth video conferencing with a physiotherapist is great for ANYONE who cannot get to the clinic in person.
Examples include:
- People who have mobility or transportation restrictions
- Living remotely with no clinic nearby
- Caregivers with dependents or new babies at home
- People who are at work and cannot leave the office
- Stuck by inclement weather
- Services you need are not available through a local physio
What services can Telehealth physio offer?
Physiotherapy services through Telehealth include:
- Orthopaedic injuries, conditions, traumas
- Pelvic Health
- Exercise prescription and programming
- Clinical Pilates
- Corrective taping
- Pre-op Rehab
- Post-operative Rehab
- Self release and Mobilization
- Temporomandibular joint conditions
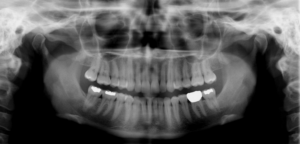
Temporomandibular Joint Dysfunction (TMD)
TMJ means Temporomandibular Joint, which is the joint where your lower jaw connects to your facial bones just in front of the ear. Disorders of this joint can lead to symptoms such as joint clicking/cracking, popping in the ear, ear pain, facial pain, numbness and tingling in the face or tongue, excess salivation, sinus congestion, headaches, neck dysfunction, and dizziness to name a few. Clients can also complain of difficulty chewing, reduced mouth opening, mal-tracking jaw, teeth that do not touch uniformly when biting down, grinding the teeth, and clenching.
TMJ disorders can be related to injury/trauma, stress/anxiety, dental work, and neck dysfunction.
Physiotherapy treatment for TMJ Disorders includes postural examination and correction, and may include a combination of manual therapy to the chewing/biting muscles and those in the neck and covering the head, mobilization of the facial bones, jaw and neck, acupuncture as tolerated, electrical stimulation, and therapeutic exercises.
Often success for this type of disorder can be improved by an interdisciplinary approach between physiotherapy, dentistry, and chiropractic care.